Knee replacements are becoming increasingly common for individuals between 55-85 years old. Approximately 1 million knee replacements are done per year in the United States with an increase to 3.5 million to occur by year 2023. Knee replacements are considered one of the most successful surgeries known due to patient satisfaction rate and low complications for patients.
Total knee replacement patients can achieve a pain free knee after successful rehab post total knee replacement surgery. Joint replacement surgery is a great option to rid of persistent knee pain, knee arthritis, and chronic pain.
Knee osteoarthritis, or the infamous “wear and tear” or “bone on bone”, is responsible for knee pain, muscle weakness and poor balance - all of which can cause falls and poor safety with activities of daily living. A total knee replacement (or a partial knee replacement) can improve all of this. A common complaint many patients have after the total knee replacement surgery is the knee feeling “not like my knee”. There are various reasons why this occurs all of which are explained below.
Proprioception
Proprioception is a word to describe how our body moves in space. Here's an example to give you a better understanding. Close your eyes. Put your hand out in front of you. How did you know your hand was out in front of you if your eyes are closed? Well, the joint in the body communicate with the brain to tell you where your body is. Pretty cool!
As we age, our proprioception decreases causing us to have less coordination and balance. If you add age and arthritis into the equation, your proprioception will be very poor. Before a knee replacement, the structures inside the knee joint are worn down due to arthritis or injury. This causes the proprioception to worsen. We have less control of our knee joint, the muscles don't contract properly when we move in various directions, balance changes. Proprioception is responsible for coordination, injury prevention, fluid movements, motor control, balance, etc. Proprioception helps our movement feel normal.
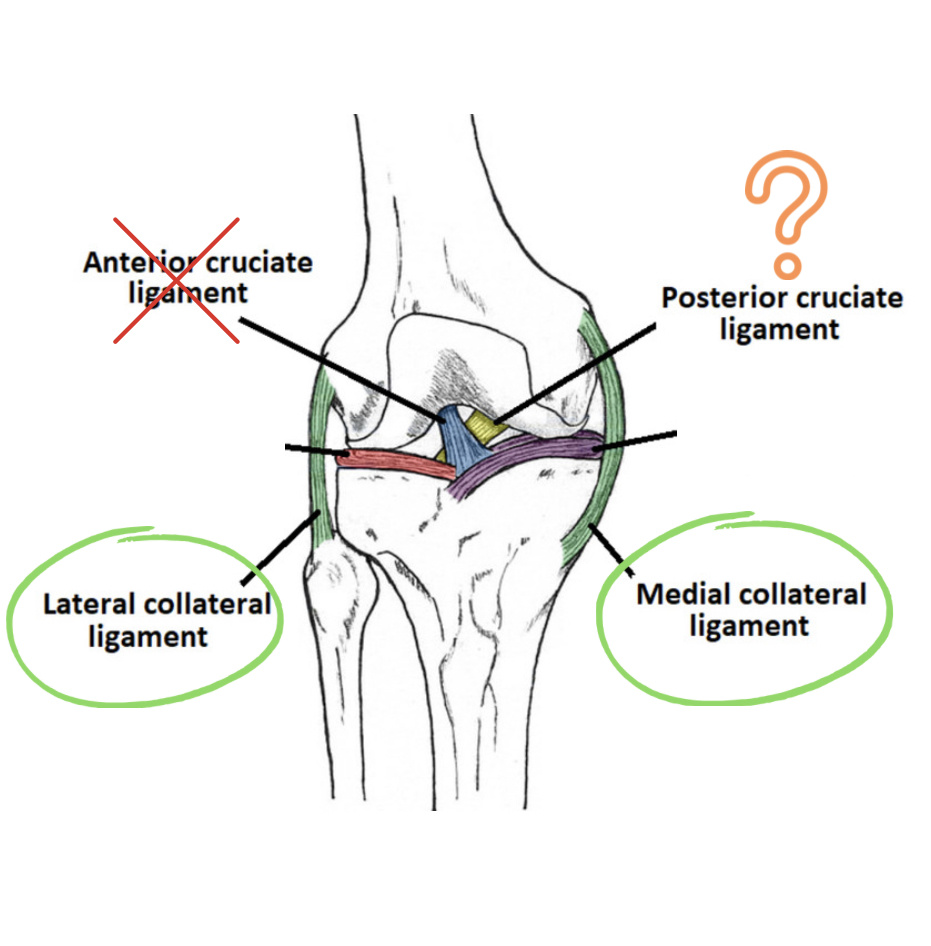
All of the ligaments and meniscus in the knee are responsible for proprioception. During a knee replacement, the ACL and meniscus are removed causes an immediate hit to proprioception of the knee joint. However, the LCL, MCL and sometimes the PCL is reserved, which helps the knee feel and act more like a “real knee.” New procedures are emerging where surgeons are preserving all the ligaments including the ACL, but this is a specialized surgery reserved for athletes.
Not only do the ligaments have receptors in them, but the muscles and tendons also have receptors in them that communicate with the brain to provide coordination and balance feedback. This is a good thing to recognize because it allows the body to recover its proprioception even after a joint has been replaced.
Muscle Strength
After the knee replacement surgery, the muscles become very weak due to many reasons. Prior to knee replacement surgery, it is very common to have weakness due to disuse, meaning we tend not to use our leg that hurts. For most people, the muscle that takes the biggest hit is always the quadriceps muscle. The quad muscle is very important for overall daily activities. It allows us to get off of chairs, to walk, to stand for long periods of time, and the list goes on.
During surgery, the quadriceps muscle will be injured. The doctor will cut the muscle (unless you are having a quad sparing surgery) to get to the knee joint. The cutting of the quad muscle causes a lot of post surgical weakness and pain. It takes the body 6-10 weeks to fully heal a muscle tear; however, it is not recommended to wait 6-10 weeks to do quad strengthening exercises. Low intensity quad strengthening exercises should begin right after surgery with the intensity of strengthening getting more difficult as tolerated by the patient.
During surgery, the quad muscle also will lose blood flow and oxygen from the tourniquet placed on the thigh. This causes significant weakness in the leg. Some surgeons use a tourniquet for over 30 minutes on the thigh to control blood loss and allow for a cleaner working area when cementing the knee replacement in.
If the surgery is more complicated, the tourniquet could be on the thigh/quad for even longer. OUCH. But in general, the tourniquet is placed for 18-28 minutes. It is possible that you did not have a tourniquet placed on your thigh and in that case, you will have less quad damage and less quad pain. Not using a tourniquet does come with its risks.
Advantages of tourniquet:
- less blood loss
- cleaner working area for surgeon
- more visibility
Disadvantages of tourniquet:
- quad weakness post surgery
- quad pain post surgery
- bruising
Range of Motion
If you had or are looking into getting a knee replacement, your range of motion will be a very hot topic of discussion between you and your physical therapist and surgeon. They will constantly check to make sure you are progressing with your knee bending and knee straightening. The knee will be very stiff and swollen for several months after surgery, which will limit your ability to bend and straighten the knee. Not only does swelling limited your range of motion, but scar tissue after surgery will also cause limitations. It will feel very tight when you do your physical therapy stretches and often times, this sensation causes a lot of frustration and discomfort.
Between 6-12 weeks, your range of motion should be at or very near full capacity. You should have a completely straight knee (0 degrees) and a knee that can bend fully (115-130 degrees). Once you reach your full potential with your range of motion, your knee will feel less stiff, achy and tight throughout the day. Your physical therapy exercises will help you achieve your range of motion goals.
Tips to Improve Range of Motion
- Don’t use ice packs before stretching
- Warm up (walking or PT exercise) prior to stretching
- Use bike before stretching
- Take pain medication as prescribed
- Perform stretches as prescribed by Physical therapy
- Take deep breaths during initial discomfort with stretches
When will my Knee Replacement Feel Normal
With all the changes after a knee replacement, your knee will take some time to get used to the changes. Your recovery process will be
- 25% by one to three months: at this time, you will have significant swelling, knee pain and discomfort. Sleeping will be challenging. You should expect increased pain at the end of the day, stiffness and soreness. Taking pain medications is expected.
- 50% by three to six months: most patients have improving symptoms. Less soreness and knee pain throughout the day. You should expect stiffness and aching especially after a long day of activity. Taking over the counter medications is expected.
- 90% by six to nine months: your new joint will less sore and stiff. You will be able to get through a long walk without feeling like you have a knee replacement.
- 100% by twelve to sixteen months: Both knees should feel adapted to this new prosthesis. You might have an occasional twinge if you do too much or with certain activities. Overall, you should be happy with your knee replacement surgery and be able to return to normal life.
If you have had a partial knee replacement, this process will be much faster with full recovery around 3-6 months.

.avif)









